 Because of my son’s failure to thrive, our pediatrician sent us to see Vicki Kobliner, a holistic nutritionist, who’s also on the board of Epidemic Answers with me.
Because of my son’s failure to thrive, our pediatrician sent us to see Vicki Kobliner, a holistic nutritionist, who’s also on the board of Epidemic Answers with me.
Given that Crane Man has constant fatigue and stomach pain, poor growth, mild sensory issues and developmental delays, Vicki suggested having preliminary tests for mitochondrial dysfunction done. Checking the levels of carnitine, lactic acid, pyruvic acid, alinine and lysine are easy preliminary screening tests that can be done from a standard blood-test lab like Quest Diagnostics.
Having symptoms across 3 or more organ systems is suggestive of mitochondrial dysfunction.
- Crane Man’s developmental delay is a symptom of brain dysfunction;
- His GI problems and former acid reflux are symptoms of muscular dysfunction;
- His possible hypoglycemia is a symptom of liver dysfunction;
- His failure to thrive, fatigue and former unexplained vomiting are symptoms of system dysfunction.
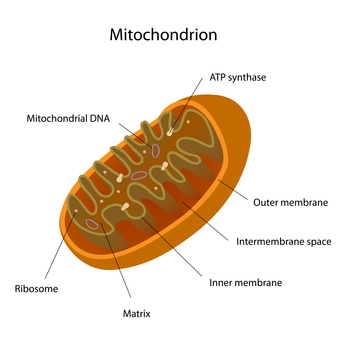
At this point, you’re probably scratching your head, thinking “Mitochondria… I vaguely remember something about that from high school biology class.” Mitochondria are the powerhouses of the cells. They make energy from our food, and if they are gunked up or damaged, they don’t work properly, and you feel tired, shaky, sick, etc.
Dr. Doug Wallace, director of the Center of Mitochondrial and Epigenomic Medicine at the Children’s Hospital of Philadelphia, says that energy is life and that all disease has its roots in mitochondrial dysfunction. You can read about him here and also in this research report he wrote for the journal Genetics: “Mitochondria as Chi”.
The College of American Pathologists says that, “Mitochondrial dysfunctions are the Willy Lomans of disease—difficult to fathom, easy to overlook, dropping hints that don’t quite add up to a full portrait.” Their article here gives a great overview of what mitochondrial disease is and why it’s so difficult to pin down.
The best way to think of mitochondrial dysfunction is like thinking about economics: supply and demand. People with mitochondrial dysfunctions can’t supply enough energy to meet their bodies’ demands. Seemingly typical things to most people can cause an energy drain in these people.
Here are some common causes of energy drains:
- Stress
- Being in a noisy, crowded environment
- Emotional stress
- Hypoglycemia
- Heat and humidity
- Too-cold temperatures
- Hormonal fluctuations
- Illness
- Too much physical activity
- Demands of school (a lot of fine-motor activity, writing, etc.)
Crane Man and My Older Son Likely Have Functional Mitochondrial Dysfunction
Crane Man’s total carnitine level was at 12umol/L; the lowest normal level is 32. Free carnitine was 10; the lowest normal level is 25. Carnitine is a conditionally essential amino acid that’s used to transport fatty acids into the cell to be used as fuel for energy production.
It comes from the Latin word “carne”, which means flesh, and, indeed, beef and pork are excellent sources of it. Not having enough carnitine means there aren’t enough conveyor belts for fuel into the cells.
Mitochondrial dysfunction causes an overabundance of metabolic by-products, high levels of which are red flags for mitochondrial dysfunction: lactic acid, pyruvic acid, alinine and lysine. Crane Man’s lactic acid level was 8, which was in the normal range of 4-16mg/dL, so there was no problem there with him.
An over-accumulation of lactic acid, as many athletes know, causes muscle cramps and spasms. From what I understand, lactic acid will increase significantly when a person with mitochondrial dysfunction is ill.
However, Crane Man’s pyruvic acid level was high at 1.63; the high normal range is 1.50mg/dL, so that is a definite red flag.
There was a mis-communication with the lab, and the wrong test was ordered for his alinine and lysine levels. Given that he had at least 15 vials taken for his regular blood panels and these newer tests, I decided to forego having him tested for these other amino acids at this time, especially since his carnitine and pyruvic acid levels suggest he may have mitochondrial dysfunction.
Imagine my shock when these preliminary tests suggested Crane Man has mitochondrial dysfunction. Let me be clear here and say that I am not talking about the classical, rare, neurodegenerative disease but rather what’s called a “functional mitochondrial disorder”, as Dr. Richard Boles talks about here and here.
It makes sense that Crane Man has an energy imbalance because his weight-percentile decline coincided perfectly with his going to preschool. In other words, he stopped gaining weight at his typical rate once he started preschool 2 years ago even though he was eating about the same amount of food.
I’m wondering if just the emotional stress of being separated from me and being in a new environment were more stress on him than he could handle. Poor baby!
Once I found out that Crane Man likely has mitochondrial dysfunction, I immediately requested tests for my older son, who has borne the brunt of the health problems between the two of them, such as more-severe sensory processing dysfunction, acid reflux, asthma, allergies, eczema, developmental delays, fatigue and hypotonia.
When he was little, my older son was so limp that he was like a limp Raggedy Andy doll. My older son’s tests also indicate he may have mitochondrial dysfunction, as his carnitine level is below the normal range at 20 and his lactic acid level is above the range at 17. No wonder he often wakes up with muscle cramps.
Notice that I said “preliminary tests”. That’s because these results cannot confirm a diagnosis. They are only screening tests for the next level of tests, such as muscle biopsy and genetic screening, that can be used to make a diagnosis, which can be tricky and elusive.
Given that muscle biopsy is painful, expensive ($15,000), invasive and requires anesthesia, which is a significant concern in kids with mitochondrial dysfunction, and given that genetic testing is expensive ($5,000), at this point, I’m not going to pursue a true diagnosis.
The only case (I think) in which I’d need to have further testing done is if Crane Man’s fatigue or other problems become so bad that I would need an IEP (Individualized Education Plan) to basically force his school to accommodate his special needs, such as more frequent foods, needing to lie down and rest, staying out of the hot sun or staying inside if it’s too cold outside for him.
In maternally inherited mitochondrial disease, mothers are also affected. I am definitely going to get myself tested because I have had many of these problems ever since I was a teenager:
- Getting overstressed by noisy, crowded environments (so why did I move to New York City?)
- Inability to tolerate heat (so why did I live in Baton Rouge and New Orleans for so long?)
- Hypoglycemia
- Lack of stamina
- And now, I’m finding out that I have pancreatic insufficiency, which can be caused by mitochondrial dysfunction.
What Causes Mitochondrial Dysfunction?
Mitochondrial dysfunction can come from genetic inheritance or exposure to environmental toxins, medications or other triggers. If it’s inherited, it can come from mom (which is known as maternal inheritance) or it can be autosomal recessive and be inherited from both mom and dad. Again, this is another reason why I want to get myself tested.
Dr. Sherry Rogers, author of books such as “Detoxify or Die” and “Is Your Cardiologist Killing You?” believes that mitochondrial damage comes mostly from environmental toxins such as plasticizers, pesticides, heavy metals, etc.
She states that when mitochondria develop leaky membranes, this is “the basis for all disease” because “the very essence of life (energy from food) is created in the mitochondria.” You can read some of the research reports blaming mitochondrial damage for diseases here and here.
Andrew Cutler, PhD, also believes that heavy metals, specifically mercury, cause mitochondrial damage. Dental amalgams, or “silver” fillings that are actually 50% mercury, are the largest source of mercury in our bodies today.
You can find out more about his heavy metal chelation protocol here and in his book, “Amalgam Illness: Diagnosis and Treatment: A Book on How to Cure Mercury Poisoning.” The book looks more like a thesis presentation and is a bit difficult to get through, but he’s got some great information in there.
Environmental toxins are passed from the mother to the fetus. The Environmental Working Group published a landmark report back in 2005 titled, “Body Burden – The Pollution in Newborns”. This report showed that a total of 287, and an average of over 200, toxins were found in the cord blood of newborns, meaning that they could only come from the mother.
Toxins bio-accumulate over time and across generations. Every generation along the way accumulates its own set of toxins, and the toxic burden is compounded. We’ve reached the point where the toxic burden is so high that our babies are being born “pre-polluted”, as the Body Burden report says.
I have tremendous guilt again for passing on heavy metals and other toxins to my kids. Gnashing of teeth. If only I had known to get myself tested for heavy-metal toxicity before even thinking about getting pregnant. If I only I had done proper detox for a few years before getting pregnant.
However, just so you know, it is not widely accepted by the western medicine mitochondrial community that heavy metals cause or are part of mitochondrial dysfunction, but there is increasing consensus that mitochondrial disease can be “triggered” by chemicals or physiological stress and can be made worse by alcohol consumption (especially binge drinking), cigarettes and MSG.
This meta-study, “Mitochondrial Regulation of Epigenetics and Its Role in Human Diseases”, looks at a number of studies that look into how toxins can damage mitochondrial DNA or even nuclear DNA, leading them to trigger diseases for which a person may be predisposed.
Classically trained geneticists believe that mitochondrial disease is inherited maternally (there are 13 known dysfunctions: POLG, LHON, MELAS, etc.) or is autosomal recessive (one from the mother and one from the father).
Historically, these were thought to be rare and neurodegenerative, so this is the basic thinking of MOST mainstream, western medicine geneticists: that mitochondrial disease is rare and that you cannot stabilize these people.
But because of what we have learned from others (Dr. Boles, Dr. Wallace, Dr. Haas, Dr. Rogers, Dr. Cutler and more) this thinking may soon change. They believe that mitochondrial dysfunction is not “rare”. They believe it’s really quite common because it has its roots in MANY illnesses today.
What Conditions Are Associated with Mitochondrial Dysfunction?
Mitochondrial dysfunction can cause a host of symptoms:
- Seizures
- Lack of energy, low stamina (Crane Man, my older son and myself)
- Failure to thrive (Crane Man and my older son)
- Muscle pain, spasms and cramping (my older son)
- Muscle weakness (my older son)l
- Memory and concentration issues
- Heat intolerance (Crane Man, my older son and myself)
- Developmental delay (Crane Man and my older son)
- Lack of coordination (Crane Man, my older son and myself)
- Constipation
- Reflux (Crane Man and my older son)
- Slow motility, gastroparesis (Crane Man)
- Nausea
- Migraines/headaches
- Dizziness
- Malabsorption (Crane Man, my older son and myself)
- Immunodeficiency (Crane Man, my older son and myself)
- Sleep issues and dysfunctions (my older son and myself)
- Difficulty recovering from fever, illness or anesthesia (Crane Man)
- Pancreatic insufficiency (now you can see why I want to get myself tested for mitochondrial dysfunction!)
You can also see why Vicki wanted to have Crane Man tested given his lack of energy, failure to thrive, heat intolerance, developmental delay, reflux history and abdominal pain.
In fact, about 6 months ago Crane Man seemed to have a sudden onset of chronic stomach pain. We thought at the time that his runny nose was causing mucous to upset his stomach, but what may have happened was a “mito crash”.
Illness and stress of any kind (even if you think it’s no big deal) can place a huge energy drain on a body that has trouble supplying it, and the body “crashes” with symptoms like fatigue, pain, nausea, GI system shutdown, etc. His energy level has never quite recovered since that time.
Who Is At Risk for Having Mitochondrial Dysfunction?
Mitochondrial dysfunction is common in people with:
- Developmental delays (Hmm, both of my sons had this…)
- Autism
- PDD-NOS
- Sensory processing/integration dysfunction (Hmm, both of my sons had this, too…)
Given the overlap of conditions, symptoms and people that most likely have it and given that mitochondrial dysfunction can be caused by environmental toxicity, I’m wondering if it has anything to do with methylation defects that I blogged about recently.
Methylation defects are common in people with autism, ADHD, allergies, asthma, sensory processing dysfunction, autoimmune diseases and more.
A methylation defect means that you’re not able to detoxify properly, and, in fact, toxins typically pile up, leading to a whole host of symptoms, conditions and diseases similar to what’s seen in people with mitochondrial dysfunction.
Hmm. I haven’t seen any research discussing the overlap between the two, but that doesn’t mean that there aren’t any reports. Please let me know if you’ve seen any!
What Can We Do About Mitochondrial Dysfunction?
People with mitochondrial disease usually take what’s known as the “mito cocktail”. It’s a mix of vitamins, minerals and other nutrients that are given at therapeutic doses to boost a person’s energy level.
A first line of supplementation usually contains CoQ10, carnitine and creatine, riboflavin (B2) as well as other B vitamins, and an antioxidant component of vitamins C and E. Some MD’s also use thiamine, alpha lipoic acid, folinic acid and selenium.
Visit this link at UMFD.org to see what tier one and tier two supplements are frequently used to treat mitochondrial disorders but be aware that each person’s cocktail tends to vary based on symptoms, labs and supervising physician.
Vicki recommended that we start with an over-the-counter supplement of carnitine as well as CoQ10 and increasing his B vitamins.
If you’ve read my blogs before, you probably realize that I already give my kids quite a cocktail of these nutrients already. This practice started when we started seeing a naturopath, who prescribed basics like probiotics, fish oil, minerals, etc. So, luckily this wasn’t something new to us. However, it obviously wasn’t enough to make a big difference.
The difference came when the kids started taking a prescription called Carnitor; the generic is called levocarnitine. They tried the OTC carnitine that Vicki initially recommended, but it didn’t seem to make a difference. Oftentimes, it’s not bioavailable enough or potent enough to make a difference.
With the help of Vicki, who works with kids on the spectrum, as well as kids with ADHD, SPD, etc., we were able to convince our pediatrician who was completely unfamiliar with Carnitor to prescribe it. And, wow, what an immediate difference, especially in Crane Man.
Crane Man no longer lies on the floor so much sucking his fingers because he’s so tired. That’s not to say that he doesn’t do that anymore, but he certainly does it a lot less. He’s also more active, which makes me worry me a lot less about him starting kindergarten this fall.
Personally, I think the Carnitor is great, but it’s still not enough for him. Ever since he began complaining of stomach pain about 6 months ago, he has not been as active. Maybe there was a mito crash that he never recovered from?
Given that Crane Man’s energy is still not optimal, Vicki suggested further possible supplementation with carnosine, creatine, phosphatidyl choline and possibly making further changes to his diet. She cautions against taking too many supplements, though, because they can really upset little tummies.
My older son, however, has far more stamina than he has ever had. He runs around so much outside these days that he comes in sweaty and thirsty. You may think, “Big deal”, but this is the kid who used to cry from overheating if he was left in the sun for more than 5 minutes.
He was never as physical as typical boys, which is what’s made it hard for him to relate socially with boys his age (he’s now 7). Without the Carnitor, that difference would only become more pronounced as he gets older.
I can’t wait to see how much his swimming and soccer improve. I’m so excited! In fact, the only proven treatment for people with mitochondrial dysfunction at this time is exercise, so it’s important to get kids that have some form of it moving and active, which is tough when the child is fatigued.
Dr. Terry Wahls has recovered herself from multiple sclerosis with diet, and you can see her incredible story here. She titled the talk, “Minding Your Mitochondria”, so that gives you a clue at how powerful a change this can be. She’s also written a book about how she recovered herself. I haven’t read it yet, but it’s on my wish list. You can also find Dr. Wahls and her foundation on Facebook.
Further Resources
There are some great resources out there for those wanting to know more about mitochondrial dysfunction. The first is www.mitoaction.org, which is the website for a non-profit organization whose goals are to support, educate and advocate for those with mitochondrial disease.
They “are a committee of parents, patients and clinicians from top Boston hospitals who care about improving the daily quality of life for all people affected by mitochondrial disease.”
There are also quarterly free tele-conferences for parents looking for information on the connection between mitochondrial disease and autism. This is an opportunity for families to connect with people knowledgeable about mitochondrial disease. You can find this link at www.mitoaction.org/autism.
The Executive Director of MitoAction, Cristy Balcells, wrote an excellent book called, “Living Well with Mitochondrial Disease: A Handbook for Patients, Parents, and Families”. It’s the one book you need if you want to learn about mitochondrial disease from soup to nuts.
There is a lot of excellent information available on the United Mitochondrial Disease Foundation (UMDF) website at www.umdf.org.
There are also some great Facebook groups out there where you can post questions and get responses from people who are living with this, usually in the severe form. They can tell you about specific doctors in your area, etc.
It’s also just a great way to stay connected and learn what everyone else is going through and compare it to your own journey.
I am very fortunate to have access to a very knowledgeable mom of 2 boys with more-severe cases of mitochondrial disease, which is unfortunate for them.
She was kind enough to take hours of her time to explain the differences between classic mitochondrial disease and functional mitochondrial dysfunction, how it is tested for, and what to do about it.
She even reviewed this blog for me to make sure it is technically correct, as this is something new to me, but it’s something that she’s been dealing with for her sons for many years. So, thank you; you know who you are.